External Quality Review (EQRO)
For more than 50 years, Qsource has been working with state Medicaid agencies to enhance the value of healthcare services provided to the Medicaid managed care population.
Qsource is a designated, independent External Quality Review Organization (EQRO) helping state agencies meet federal regulations for assessing managed care organizations (MCOs), prepaid inpatient health plans (PIHPs), and prepaid ambulatory health plans (PAHPs).
Qsource evaluates and aggregates information on the timeliness, access, and quality of healthcare services furnished to Medicaid enrollees as required by the code of federal regulations 42 CFR Part 438, Subpart E and Centers for Medicare & Medicaid (CMS).
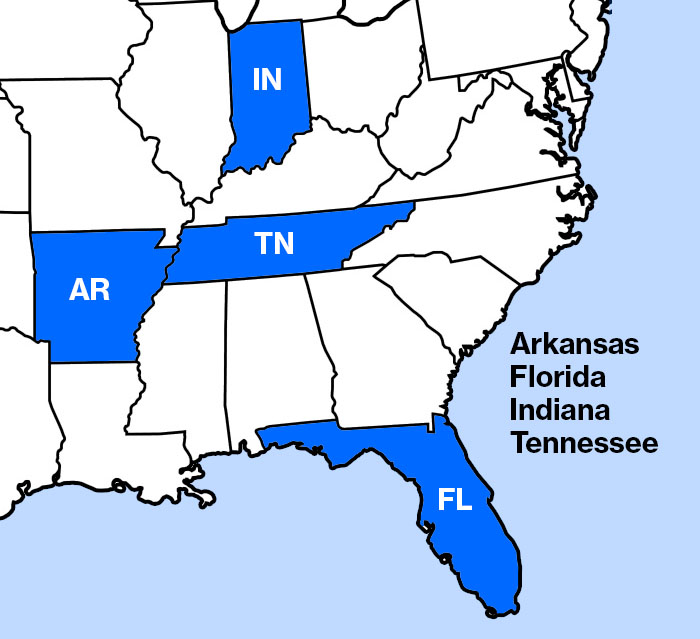
Qsource is the EQRO in four states, Arkansas, Florida- Florida Healthy Kids Corp., Indiana, and Tennessee. With our national subject matter experts, data analysts and proven processes, we know how to partner with you to improve performance.
The EQR process currently consists of four mandatory activities and six optional activities, in addition to producing an annual EQR technical report and providing technical assistance, as needed. Each of the mandatory and optional activities has a corresponding CMS EQR protocol, which Qsource follows when performing each EQR activity.
We have helped several states establish their EQR programs and have worked with them throughout their transitions to new managed care models by conducting readiness reviews and providing technical assistance and program guidance.
As an External Quality Review Organization and a QIO-like organization, we have worked with states and MCOs in virtually every area of operations and management. We use data analysis, audits and technical assistance to improve MCO and network performance.
Here are just a few of the services we have provided:
- Expertise in mandatory performance measures: reviewing for compliance, validating performance measures, performance improvement projects (PIPs), network adequacy
- Preparation of technical and annual reports
- Encounter data validation for MCO contracts
- Experience with the optional protocols requested by the States
- Customer and provider surveys
- Assistance with developing required quality strategies
- Technical assistance with quality improvement
With an in-depth knowledge of managed care systems, the Qsource EQRO Division meets EQR challenges with:
- Certified HEDIS Auditor
- Clinical QI Specialists
- Healthcare Data Analysts
- Data Engineers
- Call-Center Staff
- Technical Writers
- Epidemiologist
- Data Security standards
- HIPAA Compliant
- SOC 2 Type 2
- Annual Cloud Penetration Testing
- NIST
- Encryption
